Advances in cancer imaging: functional, molecular and AI innovation for clinical practice
The legacy of x-rays
Wilhelm Conrad Röntgen’s discovery of x-rays in 1895 revolutionized medicine. Within a year, x-rays were being used not only for diagnosis but also for cancer treatment.
Today, Consultant Clinical Oncologists in the UK are members of The Royal College of Radiologists reflecting the deep connection between imaging and oncology.
X-ray techniques are still important and routinely used, for example in breast screening mammography. However, the most exciting innovations are in non-radiation based techniques.
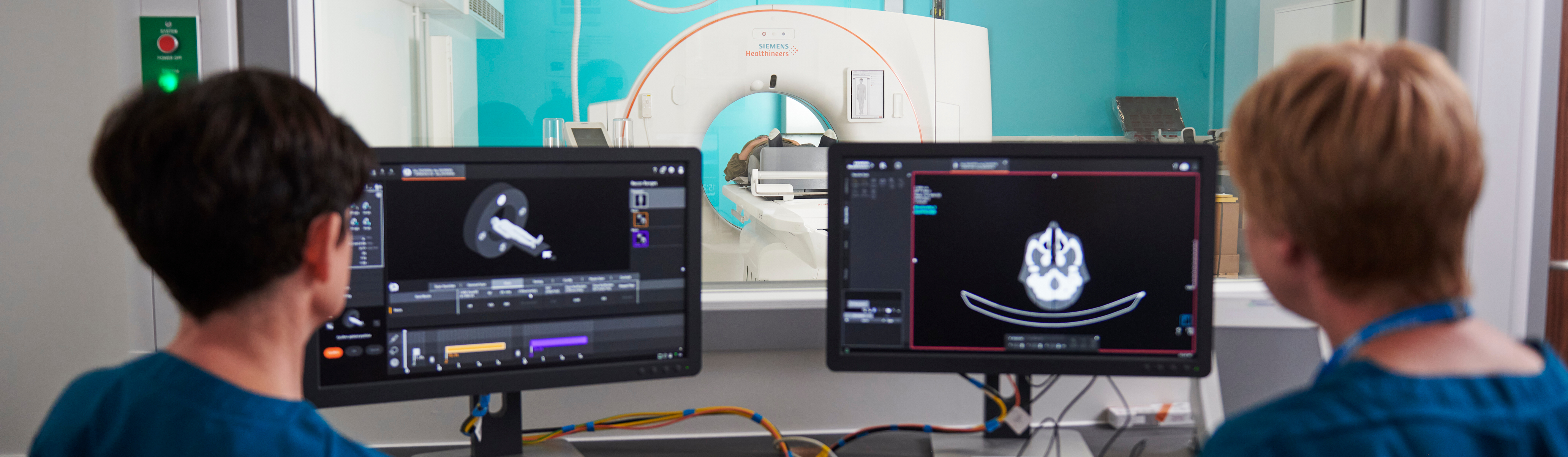
Modern imaging: CT and MRI
Standard tests like computerised tomography (CT) and magnetic resonance imaging (MRI) scanners continue to evolve. These advances have allowed routine testing to have greater sensitivity to detect smaller cancers and better specificity to tell the difference between malignant disease and benign changes.
These improvements produce vast amounts of data prompting global efforts to use Artificial Intelligence (AI) to help with scan reading. Including lung cancer CT, prostate MRI scans, and mammograms.
Functional and Molecular Imaging
Traditional imaging focuses on anatomy: is an organ too big? Are there shadows present where there should be none?
But cancer can affect our bodies without changing the size and shape of our component parts. In order to see and monitor cancer we need to be able to detect the activity of the cells – what they are doing - this is the realm of functional and molecular imaging.
Functional MRI (fMRI)
MRIs can detect small changes in the magnetic properties of blood dependent on how much deoxyhaemoglobin is present and use this factor to detect brain activity in functional MRI (fMRI).Diffusion Weighted MRI (dwMRI)
The ability of water to diffuse in and out of cells alters in abnormal tissues and this can be detected in diffusion weighted MRI (dwMRI). These scans can be used to distinguish benign from malignant tissue and have proven to be useful for investigating and diagnosing head and neck cancers and brain tumours.
Molecular Imaging and PET scans
Molecular techniques analyse various separate metabolic processes taking place inside tissue. The most widely used of these is Positron Emission Tomography (PET) scanning. PET scanners use radiotracers – safe, injectable chemicals that produce a small temporary and measurable amount of radioactivity. Different radiotracers can be developed for different use dependent on how they are taken up into different tissues. The most widely used tracer is a form of glucose (FDG). All active cells use carbohydrates like glucose in some form.
More active cells use more glucose so take up more of the tracer and are more easily demonstrated on a PET scan. Cancer cells have more active glucose consumption, so a PET scan shows them well (alongside other active tissues such as the heart and brain). This knowledge has contributed to the myth that sugar ‘feeds’ cancer. PET scans are widely used in both cancer diagnosis and in treatment monitoring but new radiotracers are extending their use.
Radiotracers
Prostate-specific membrane antigen (PSMA) is a tracer which, as the name suggests, is highly sensitive at detecting prostate cells and is becoming widespread in detection of prostate cancer after treatment. Radiotracers are now in development that have potential to monitor the very specific targets used in modern cancer drug therapies such as immunotherapy where PDL-1, PD-1 and CTLA-4 may all potentially be identified by PET. Breast cancer research has already shown that the oestrogen and HER-2 receptors that are used to select therapies can also be monitored with functional imaging and may have an important role in the future is tracking success of these therapies for individual patients.
Scanxiety: supporting patients
For people living with cancer, scans can trigger anxiety known as scanxiety..
Up to two-thirds of people experience scanxiety before cancer scans.
"I will have regular scans and, on each occasion, will be right on edge for the couple of weeks beforehand. It is just a waiting game between me and the tumour. Who is going to blink first?" Adam Blain, Pearshaped.
Support is available
If you are someone you know is struggling with anxiety of waiting for a cancer scan result then you can:
- Call the Macmillan Support Line for free on 0808 808 00 00, 7 days a week, 8am to 8pm
- Join our Online Community to connect with those who may be going through a similar experience
- Chat to us online, open 8am to 8pm, seven days a week.
Why this matters to patients
- Imaging innovations like AI-assisted CT and MRI improve diagnostic accuracy and speed, supporting timely treatment decisions.
- Functional and molecular imaging enable more personalized care by revealing tumour biology and treatment response.
- Emotional support remains critical - scanxiety affects up to two-thirds of patients, and clear communication can ease distress.
- Staying informed about these advances helps HCPs deliver holistic care that combines technical excellence with patient-centered support.
What you can do now
- Visit our HCP blog hub for expert updates on imaging, treatment pathways, and supportive care.
Share with your team
- If you work in oncology or radiology, share this blog to spark conversations about integrating imaging techniques and addressing patient anxiety.
Stay informed
- Sign up for our professional newsletters to keep up to date with the latest clinical developments and practical



