Holistic Needs Assessment (HNA)
A Holistic Needs Assessment (HNA) is an assessment and discussion you may have with someone from your healthcare team.
What is a Holistic Needs Assessment (HNA)?
A Holistic Needs Assessment (HNA) is a discussion you have with someone from your healthcare team. First you fill out an assessment or answer some questions. Then you talk through your needs and concerns with them. You both then agree on a plan for your care and support needs.
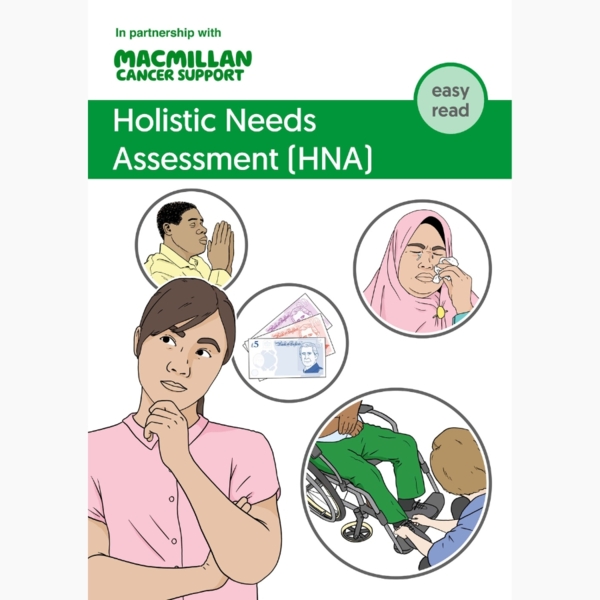
It is called holistic because you can discuss any area of your life that has been affected by cancer. An HNA is not only about the physical symptoms of cancer or the side effects of treatment.
These concerns can be:
- physical
- emotional
- practical
- financial
- spiritual.
HNAs may not be offered in all hospitals or GP practices. The HNA may happen in the ways we describe, or it may be more informal. If you are not offered an HNA and would like one, you can ask someone from your healthcare team or your GP about it.
What are the benefits of having an HNA?
Being diagnosed with cancer and coping with its effects on your life may feel overwhelming. You may have lots of questions or worries. Having an HNA can help make sure you get the support you need for these different concerns.
This may include:
- helping you identify the concerns that are most important to you
- getting information and support to help you manage your concerns – for example, side effects or support with emotional worries
- helping your healthcare team understand what is important to you
- being referred to other services if you need more help or support – for example, physiotherapy, counselling or help with your finances
- helping you to plan ahead.
What happens at an HNA?
An HNA usually has 3 parts:
- You fill in a checklist or answer some simple questions about all areas of your life – This is to find out about the concerns you may have. You are often asked to rate how important these concerns are to you from 1 to 10, with 1 being the least important and 10 being the most important. This can help you decide what to discuss first during the assessment.
- You discuss your answers with someone from your healthcare team – This is a chance to talk about the issues that are most important to you.
- You create a care plan together for managing your concerns – This is sometimes called a personalised care and support plan. If there are simple ways to help you, you may not need a written care plan.
Booklets and resources
Discussing your care
It can help to think about the concerns you would like to discuss before your HNA.
What the discussion may include
These are your concerns, so it is up to you what you talk about. Some ideas include your:
- physical symptoms – for example, pain, tiredness, bowel or bladder problems, and weight changes.
- treatment – for example, side effects, fertility, and the risks and benefits of treatment.
- emotions – for example, fear of cancer coming back or the effect of cancer on your relationships.
- sexual well-being – for for example, concerns about intimacy, getting an erection or low sex drive.
- family – for example, how to talk about cancer or worries about genetic risk.
- well-being after treatment – for example, giving up smoking, eating healthily or staying active.
- follow-up appointments – for example, tests you may need and knowing what symptoms to look out for.
- work, money and housing – for example, advice about working during treatment, benefits and financial help.
- practical issues – for example, how to manage housework, and where to get aids and equipment to help you.
- spirituality – for example, your faith or beliefs, and whether your cancer experience has affected these.
For some practical or financial issues, you may be referred to other health or social care services. These will give you further advice and support.
Remember, the concerns we have listed are only a guide. Not everything listed will apply to you. Or you may have concerns that are not listed. We have some suggestions to help you decide what you would like to discuss.
Preparing for your discussion
You may find it helpful to make notes of any concerns or questions you have before the discussion.
You may want to think about these questions:
- Are you coping okay?
- Is cancer affecting your relationships with family or friends?
- Are family or friends coping with your diagnosis?
- Would you like to know more about local services, support groups or helplines?
- Do you need advice about your diet, being physically active or stopping smoking?
- Are you confused by any part of your treatment or follow-up care? Is there anything you would like explained?
- Do you need help with finances, work or education?
- Are you worried about the future?
- Do you feel your quality of life could be improved?
- Are you having any symptoms or side effects from the cancer or treatment?
- Do you know what signs and symptoms to look out for and who to contact if you notice any?
- Do you know who to contact if you have any problems? For example, do you have the contact details of your key worker?
Not all these suggestions will be relevant to you. The HNA is about your personal needs and concerns.
Your care plan
During the discussion, you and the person doing your HNA will agree on the best ways to manage your needs and concerns. They may write down what you have agreed in a document called a care plan. This is sometimes called a personalised care and support plan.
It may be written as a letter instead. They may write it during the discussion. Or they may make notes and send it to you afterwards.
Your care plan will record:
- the main concerns you talked about
- suggestions and actions to help you manage your concerns
- services that may be able to support you, and any referrals they make
- what is already being done to help – for example, the services you are already using
- information about who to contact if you need more help
- the details of other health and social care professionals you have agreed to share the information with.
You will be given a copy of your care plan. If you are not offered a copy of your care plan, you can ask for one at any time.
A copy of the care plan may be sent or given to:
- your GP, so they know your concerns and what help is planned
- other members of your healthcare team, to help them plan or improve your care
- specialist support services – for example, a dietitian or counsellor.
The healthcare professional will only share your care plan if you give permission. They will only share as much information as people need to help with your care.
Your care plan will be securely stored with your other health records. You can ask for a review of your care plan, or a new assessment, at any time.
Who do I have the HNA with?
You may have your HNA with someone from your cancer team at the hospital. This is often your clinical nurse specialist (sometimes called your key worker). Or it could be a cancer support worker who works with them.
Or you may have your HNA with someone from your GP practice. This may be your GP, practice nurse, cancer care co-ordinator or another member of the team.
They have the skills and experience to:
- help you identify your needs
- talk about your needs with you.
They also have up-to-date knowledge of local and national services. They can refer you to other support services you may need. They may print out some Macmillan information to give to you.
If you are having a face-to-face assessment, you can take a family member, carer or friend with you. You can ask for an interpreter if you need one.
If you have not been offered an HNA, ask your healthcare team about who can do the HNA with you.
When does the HNA happen?
You may be offered an HNA when you are diagnosed, during treatment or after treatment has ended. If you are not offered an HNA, you can ask someone from your healthcare team to arrange one. Your needs may change over time, so you can ask for another HNA at any time.
You may have a separate appointment for the HNA. Or it may happen during one of your other appointments.
You may be sent the checklist of questions to answer online at home before the HNA. Or you may be asked to complete the checklist in the waiting room beforehand.
The checklist may be on paper or a handheld electronic tablet. If it is done on a tablet, it is called an electronic Holistic Needs Assessment (eHNA). If you need help answering the questions or using the tablet, tell the person doing your HNA.
Some people have their HNA as an informal discussion with someone from their healthcare team. It may not always be called an HNA. They may ask you questions and discuss your answers with you, rather than asking you to fill out a form or complete a checklist.
Where will the HNA happen?
The HNA should be done in a private and comfortable room. It may be done in the hospital or your GP practice. Or it can be done over the phone. It can also be done online in a video call (virtually). You can tell the person doing your HNA what you would prefer.
How long will the HNA take?
The HNA usually takes between 30 minutes and 1 hour. Some people need longer. It should take as long as you need to talk about your concerns.
If there are still some things you want to talk about after it has finished, tell the person doing your HNA. They can make another appointment with you.
Cancer care review
A cancer care review is a conversation with your GP, practice nurse, cancer care co-ordinator or someone else from your healthcare team. This may happen a few months after being diagnosed, or sometimes later. They will check whether you have any concerns or need any more information or support. Sometimes the cancer care review may be done as another HNA.
We have more information about having a cancer care review.
About our information
This information has been written, revised and edited by Macmillan Cancer Support’s Cancer Information Development team. It has been reviewed by expert medical and health professionals and people living with cancer.
-
References
Below is a sample of the sources used in our after treatment information. If you would like more information about the sources we use, please contact us at cancerinformationteam@macmillan.org.uk
ESMO Expert Consensus Statements on Cancer Survivorship: promoting high-quality survivorship care and research in Europe. Published: 10 August 2022. Annals of Oncology (accessed April 2023).
NHS Personalised Stratified Follow Up (PSFU) Pathway in Cancer Care. Published 2022.
Macmillan Cancer Support. Providing personalised care for people living with cancer: a guide for professionals providing holistic needs assessments, care and support planning. Published October 2019. Available from: www.macmillan.org.uk
Date reviewed

Our cancer information meets the PIF TICK quality mark.
This means it is easy to use, up-to-date and based on the latest evidence. Learn more about how we produce our information.
The language we use
We want everyone affected by cancer to feel our information is written for them.
We want our information to be as clear as possible. To do this, we try to:
- use plain English
- explain medical words
- use short sentences
- use illustrations to explain text
- structure the information clearly
- make sure important points are clear.
We use gender-inclusive language and talk to our readers as ‘you’ so that everyone feels included. Where clinically necessary we use the terms ‘men’ and ‘women’ or ‘male’ and ‘female’. For example, we do so when talking about parts of the body or mentioning statistics or research about who is affected.
You can read more about how we produce our information here.