Innovation in cancer care
We're always looking to improve care for people living with cancer. We fund pilots and services to help professionals offer new and innovative ways to deliver care and services for patients.
Stories And Media
-
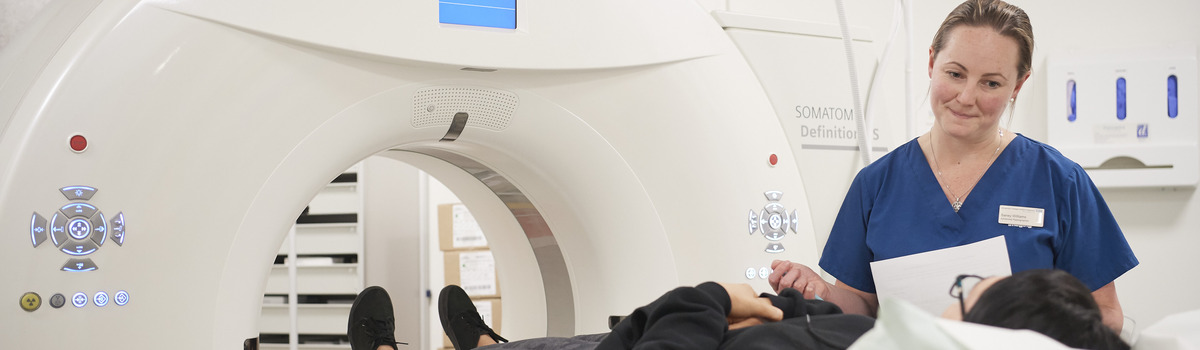
Blogs 31 Jan 2023Professor Richard Simcock, Chief Medical Officer, focuses on the power and history of imaging and its use in cancer research, diagnosis and treatment.



