Lung cancer
Choose a type
What is lung cancer?
Cancer that starts in the lung is called primary lung cancer. The lungs are the parts of the body that we use to breathe. Lung cancer is the third most common cancer in the UK. About 49,200 people are diagnosed with it each year.
In this video Dr Ranj is joined by Dr David Gilligan to take an in-depth look at lung cancer, exploring its symptoms, testing, stages and treatment options.
There are 2 main types of primary lung cancer. These are non-small cell lung cancer (NSCLC) and small cell lung cancer (SCLC). To find this out the type you have the cancer cells are examined in a laboratory by a doctor who is an expert in cell types.
Both types of lung cancer behave in different ways. Your treatment will depend on the type you have. We have more detailed information about:
There are other types of cancer that start in the lung or that sometimes spread to the lung.
Cancers that start in another part of the body, such as in the breast, bowel or bladder may sometimes spread to the lungs. This is called secondary lung cancer. We have more information about secondary lung cancer.
A cancer that affects the pleura, which is the covering of the lungs, is called pleural mesothelioma. We have more information about pleural mesothelioma.
A rare cancer that can start in the lungs is called a neuroendocrine tumour. We have more information about neuroendocrine tumours.
Related pages
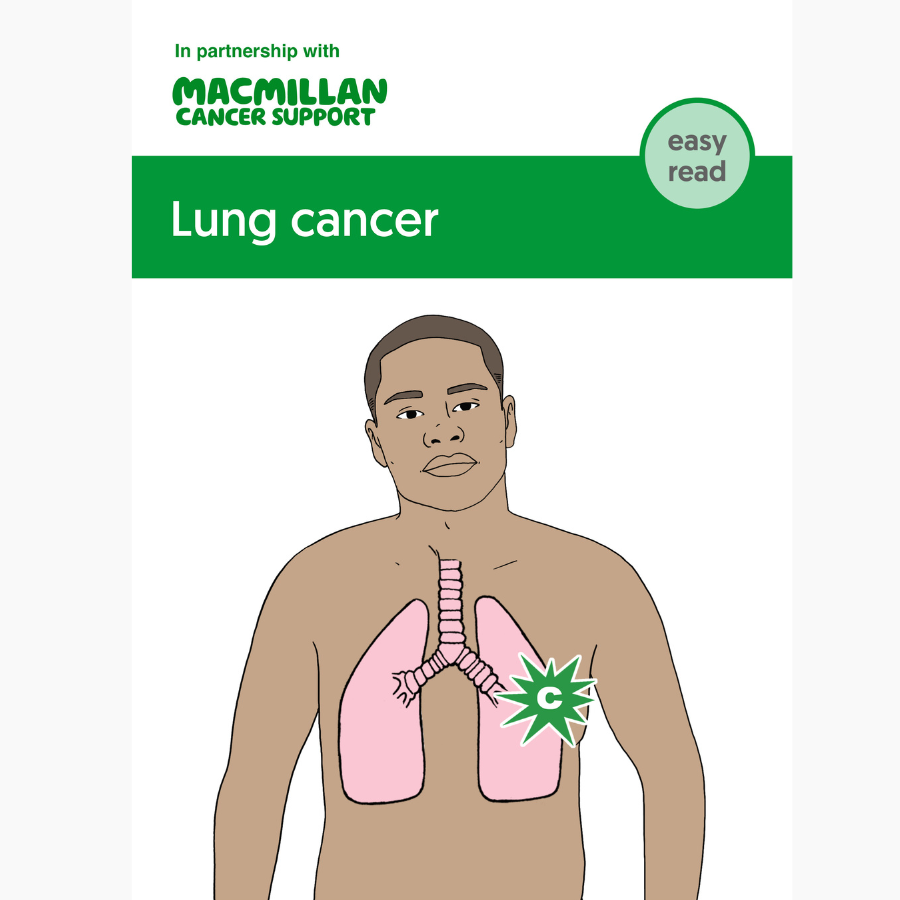
Booklets and resources
Symptoms of lung cancer
Some of the common symptoms of lung cancer are a cough for 3 weeks or more, breathlessness, or a chest infection that does not get better. These symptoms can be caused by other lung conditions or by smoking. But it is always important to get them checked.
We have more information about lung cancer symptoms.
Related pages
Causes of lung cancer
Smoking tobacco is the cause of most lung cancers and the biggest risk factor. This includes smoking cigarettes, cigars and pipes.
Some people who have never smoked can also get lung cancer. Around 15 in 100 people (15%) diagnosed with lung cancer are people who have never smoked. This is known as non-smoking lung cancer.
We have more information about the causes and risk factors of lung cancer.
Related pages
Diagnosis of lung cancer
If you have symptoms, you will usually begin by seeing your GP, who will examine you. If they think that your symptoms could be caused by lung cancer, they will arrange a chest x-ray or might refer you to a chest doctor urgently.
For some people, lung cancer is diagnosed after they have been admitted to hospital as an emergency. This may be when the cancer is more advanced and causing serious symptoms or complications. Sometimes lung cancer might be diagnosed through screening to diagnose people at risk of lung cancer at an early stage.
At the hospital a specialist nurse or doctor will examine you and talk to you about the tests you need. Tests may include:
-
Chest x-ray
If you have not already had one, you may have a chest x-ray to check your lungs.
-
CT scan
Most people have a CT scan. If you have certain symptoms, you might have a CT scan, even if your chest x-ray is normal.
-
PET-CT scan
You may have a PET scan and a CT scan together. PET-CT scans give more detailed information about the part of the body being scanned.
-
Biopsy
You usually have a biopsy to find out for certain if you have lung cancer. During a biopsy, a doctor or nurse takes samples of cells or tissue from the abnormal area to check for cancer cells. Your cancer doctor or nurse will talk to you about the type of biopsy you will have. There are different ways of taking biopsies for lung cancer. These include:
- Bronchoscopy and biopsy
- CT scan and biopsy
- Lung biopsy through the skin
- Endobronchial ultrasound scan (EBUS) biopsy
- Endoscopic ultrasound (EUS) biopsy
- Biopsy of neck lymph nodes
The results of the biopsy tell your doctor if there is cancer and the type of lung cancer that you have.
Waiting for test results can be a difficult time, we have more information that can help.
Further tests for lung cancer
Your specialist usually arranges further tests to find out more about the size and position of the cancer and whether it has spread.
-
Mediastinoscopy
A mediastinoscopy is sometimes done instead of an EBUS or EUS. It lets the doctor look at the area in the middle of your chest (the mediastinum) and nearby lymph nodes. You have it under a general anaesthetic.
-
Thoracoscopy
A thoracoscopy lets the doctor look at the lining of the lungs (pleura) and take a biopsy of the pleura.
-
MRI scan
An MRI scan uses magnetism to build up a detailed picture of areas of the body. Doctors may use it to find out the size of a cancer and whether it has spread.
Tests on lung cancer cells
Related pages
Staging of lung cancer
The results of your tests help your doctors find out more about the size and position of the cancer and whether it has spread. This is called staging. Knowing the stage and grade helps your doctors plan the best treatment for you. We have more information about lung cancer staging.
Treatment for lung cancer
A team of specialists will meet to discuss the best possible treatment for you. This is called a multidisciplinary team (MDT).
Your doctor or cancer specialist or nurse will explain the different treatments and their side effects. They will also talk to you about things to consider when making treatment decisions. You will need this information before you give your permission (consent) to have any treatment.
Treatment for lung cancer will depend on the type of lung cancer you have. You can read more in our information on:
You may have some treatments as part of a clinical trial.
After lung cancer treatment
You will have regular check-ups during and after your treatment. Some people may be on treatment for months or years if it is working well for them.
You might have CT scans or chest x-rays as part of your follow up. Appointments might be in person, or by phone or video.
Tell your doctor or specialist nurse as soon as possible if you have any problems or notice new symptoms between appointments.
We have more information about follow-up care after treatment.
Support after lung cancer
People often have many different feelings when they finish cancer treatment. You may feel relieved that treatment has finished, but worried about what will happen in the future.
We have information below about some of the things people ask about after cancer treatment. But you may have other questions or need information about something else.
Macmillan is here to support you. If you would like to talk, you can:
- Call the Macmillan Support Line on 0808 808 00 00.
- Chat to our specialists online.
- Visit our lung cancer cancer forum to talk to people who have been affected by lung cancer, share your experience, and ask an expert your questions.
Other organisations who offer information and support
-
ALK Positive UK
Provides support and advocacy and aims to improve the survival and quality of life of ALK positive lung cancer patients in the UK.
-
EGFR Positive UK
Provides support and advocacy and aims to improve the overall survival and quality of life of EGFR positive lung cancer patients across the UK.
-
Roy Castle Lung Cancer Foundation
Provides information and practical and emotional support for anyone affected by lung cancer.
Sex life
Fertility
Well-being and recovery
It can take time to recover after lung cancer treatment. Some days you may feel better than others.
A healthy lifestyle can help speed up your recovery. Even small lifestyle changes may improve your well-being and long-term health.
Even if you already have a healthy lifestyle, you may choose to make some positive changes after treatment. We have more information on leading a healthy lifestyle after treatment.
It is important to know where to get support or information if you need it. People often need support even some time after lung cancer treatment. But sometimes it is difficult to know who to ask for help. To find support:
- ask your GP or someone from your cancer team for advice about support in your area
- search cancercaremap.org to find cancer support services near you
- call us free on 0808 808 0000 or talk to us online - our cancer information and support specialists can offer guidance and help you find what you need.
About our information
This information has been written, revised and edited by Macmillan Cancer Support’s Cancer Information Development team. It has been reviewed by expert medical and health professionals and people living with cancer.
-
References
Below is a sample of the sources used in our lung cancer information. If you would like more information about the sources we use, please contact us at informationproductionteam@macmillan.org.uk
National Institute for Health and Care Excellence (NICE). Lung cancer – Diagnosis and management. Clinical guideline 2019. Last updated 2023. (accessed Nov 2023) Available at: https://www.nice.org.uk/guidance/ng122
European Society for Medical Oncology (ESMO). Small-cell lung cancer: ESMO clinical practice guidelines for diagnosis, treatment and follow-up. 2021. (accessed Nov 2023). Available at: https://www.esmo.org/guidelines/guidelines-by-topic/esmo-clinical-practice-guidelines-lung-and-chest-tumours/small-cell-lung-cancer
European Society for Medical Oncology (ESMO). Early and locally advanced non-small-cell lung cancer (NSCLC): ESMO clinical practice guidelines for diagnosis, treatment and follow-up. 2017. eUpdate 01 September 2021: New Locally Advanced NSCLC Treatment Recommendations (accessed Nov 2023) Available at: https://www.esmo.org/guidelines/esmo-clinical-practice-guideline-early-stage-and-locally-advanced-non-small-cell-lung-cancer
European Society for Medical Oncology (ESMO). ESMO expert consensus statements on the management of EGFR mutant non-small-cell lung cancer. 2022 (accessed Nov 2023). Available at: https://pubmed.ncbi.nlm.nih.gov/35176458/
Date reviewed

Our cancer information meets the PIF TICK quality mark.
This means it is easy to use, up-to-date and based on the latest evidence. Learn more about how we produce our information.
The language we use
We want everyone affected by cancer to feel our information is written for them.
We want our information to be as clear as possible. To do this, we try to:
- use plain English
- explain medical words
- use short sentences
- use illustrations to explain text
- structure the information clearly
- make sure important points are clear.
We use gender-inclusive language and talk to our readers as ‘you’ so that everyone feels included. Where clinically necessary we use the terms ‘men’ and ‘women’ or ‘male’ and ‘female’. For example, we do so when talking about parts of the body or mentioning statistics or research about who is affected.
You can read more about how we produce our information here.