Cancer diagnosis
We have information about the different tests and scans that you might have if you're worried about cancer. We also have help, practical advice and information to help you understand your diagnosis.
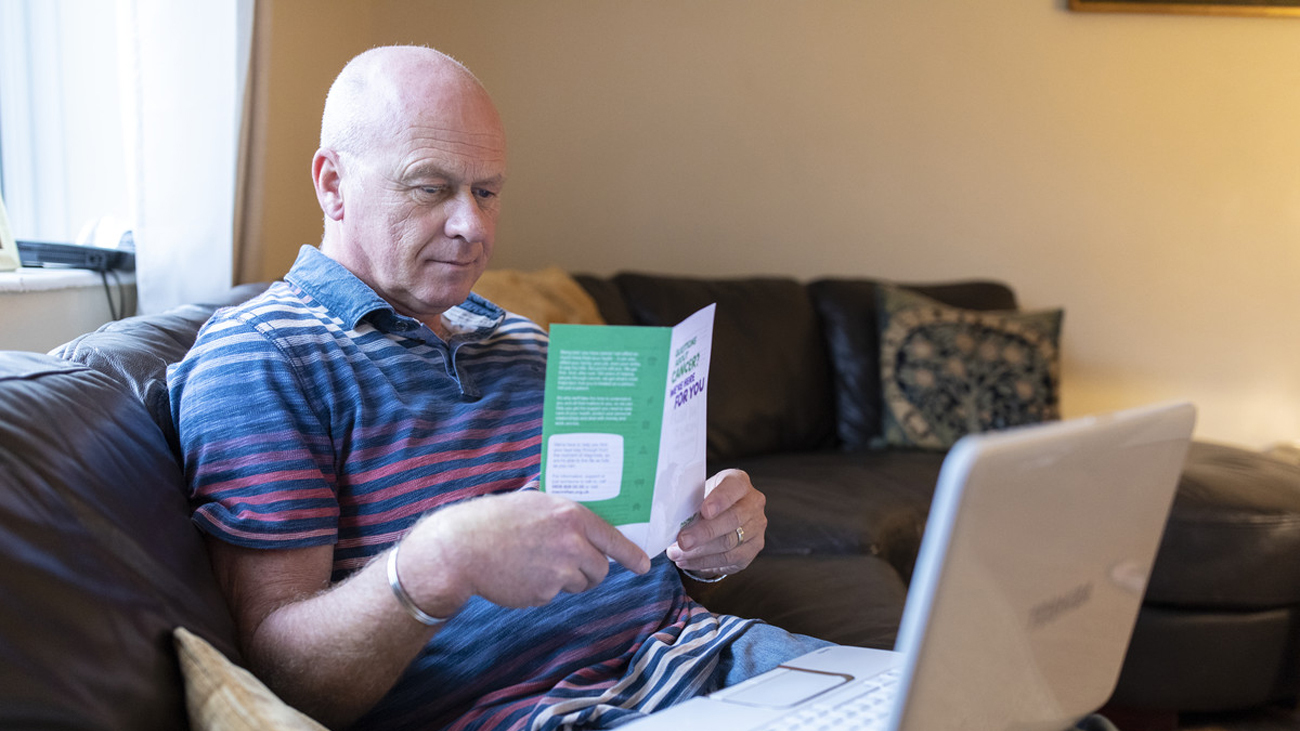
Personalised information and support
Answer a few quick questions to find the right support for you. We have information about cancer and support services, including help with money and work.